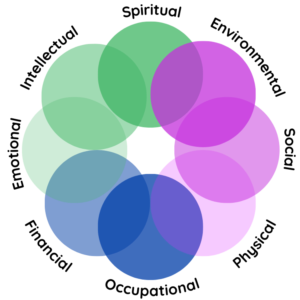
Wellness Wheel
8 Dimension Wellness Wheel
The 8 Dimension Wellness Wheel is a holistic model that assesses an individual’s overall well-being across different areas of life. It recognizes that well-being extends beyond physical health and encompasses various dimensions, including emotional, mental, social, environmental, spiritual, and occupational dimensions.
Each dimension plays a vital role in our overall wellness and requires attention and nurturing for a balanced and fulfilling life.
Environmental
Environmental
Your environment and the greater global environment play a role in your wellbeing. How you understand it, interact with it and feel its impact contribute to how you live.
Consider these:
· I care for and respect my environment and community.
· I am aware of the risks within my environment and make adjustments to protect myself from those risks
· I enjoy taking care of my living space and creating a positive place to be.
Social
Social
Your social wellness relates to the people with whom you spend time and the community in which you find yourself. Your connection and communication with others have a remarkable impact on your wellness.
Consider these:
· I maintain healthy relationships and boundaries with myself and others.
· I feel I belong to a group or community and do not feel isolated.
· I respect others and ways we are different.
· I am able to resolve conflicts in my life.
Physical
Physical
There are a lot of elements that make up your physical wellbeing: nutrition, exercise, rest, strength, endurance... you’re probably well-acquainted with most of them.
Use these ideas to assess this part of your wellness wheel:
· I get adequate sleep and I wake feeling rested.
· I eat regular nutritious meals
· I participate in physical activity each week.
· I visit with my primary care doctor regularly
Occupational
Financial
Financial
This dimension takes into account how you manage your money and how you balance your work and leisure time.
Consider these:
· I have developed a financial plan and have a balance between spending and long-term saving.
· I budget my spending each month.
· I balance work and other areas of my life.
Emotional
Emotional
This dimension helps us assess how well we’re taking care of our feelings, managing, identifying and fully engaging with them. Your emotional health often also dictates how you’re able to handle challenges that arise.
Consider these:
· I’m able to ask for/seek help when I need it – from
friends, family, or professionals.
· I recognize and manage stressors in my life.
· I am able to feel and label my feelings.
· I am able to express my emotions in a healthy way.
· I am able to comfort or console myself when I am
troubled.
Intellectual
Intellectual
Your intellectual well being is related to how you use your mind: how much you try to learn new things, your creativity and your critical thinking skills (which involves how you think and how you focus).
Consider these:
· I pursue mentally stimulating interests or hobbies.
· I make active efforts to continue to learn.
· I commit time and energy to personal development.
Spiritual
Spiritual
Your spiritual wellness encompasses your ability to discover purpose and meaning in your life and looks at how in touch you are with your values, morals and something bigger than yourself (like a higher power or
even humankind).
Consider these:
· I feel a personal sense of peace and wellbeing.
· I am aware of my own values and beliefs and respect the values and beliefs of others.
· I believe my life is meaningful and has direction.
· I am able to forgive others and myself and let go.
· Principles/ethics/morals provide guides for my life.